Link to your individual collections by creating a new linklist in the Navigation section of the admin.
You can then have it appear here by choosing your new linklist under Customize Theme / Sidebar.

Show 1384: Mending Mistrust–Can We Rebuild Faith in Medicine?
. Decades ago, people trusted their doctors and assumed that physicians always had the patient’s best interests in mind. That belief has faded and trust in medicine seems to be in tatters following the divisive battles of the pandemic. In this episode, we consider how doctors might rebuild faith in medicine.
Overcoming an Epidemic of Mistrust in Medicine:
Even before COVID-19, people were becoming skeptical about healthcare. Patients whose symptoms went undiagnosed and unaddressed felt that their doctors were not taking them seriously. Physicians reinforced that impression if they suggested that a problem like the extreme exhaustion experienced by people with myalgic encephalomyelitis/chronic fatigue syndrome might be psychosomatic. According to our guest, Dr. F. Perry Wilson, “The most powerful force in Medicine is trust.” It is the foundation for a therapeutic alliance in which patient and doctor can figure out what is wrong and how to make it better. Until we figure out how to rebuild faith in medicine, that kind of collaboration will be extremely difficult.
Building Trust Goes Both Ways:
Patients suspicious of their healthcare providers may withhold information that could be important for diagnosis or treatment. They may not disclose their recreational drug use, for example. Possibly, they may shade the truth more than usual when the discussion turns to alcohol or exercise. Clinicians need to have a sense that the patient is sharing the whole story, and patients need to perceive that the provider believes them and is working on their behalf.
The Problem with Motivated Reasoning:
If you are trying to make wise decisions about your own health, you need reliable evidence as the basis for those decisions. Unfortunately, a lot of the information we encounter online, in publications, or sometimes even in the clinic is tainted by the cognitive bias our guest calls “motivated reasoning.” Others have sometimes called it cherry-picking data.
Motivated reasoning is finding ways to support the arguments that we want to be true. You pick the data that conforms to your beliefs and ignore the rest. Or possibly you interpret evidence to allow yourself to explain away uncomfortable truths. This tendency is part of human nature. However, when it is brought to bear in the clinic or medical office, it undermines trust and makes it hard to rebuild faith in the practice of medicine.
Pharmaceuticals and Motivated Reasoning:
One of the arenas in which we see motivated reasoning at work is a discussion of the benefits and risks of medications. Science has come up with statistics to help analyze just how helpful a drug may be. We often refer to the Number Needed to Treat, or NNT, as one of these measures. We have observed that doctors who prescribe a lot of statins to lower cholesterol tend to rate the benefits high and downplay possible side effects.
Dietary Guidelines and Motivated Reasoning:
You can see similar motivated reasoning when you look at the history of dietary guidelines. Manufacturers of sugary, high-carb foods were able to get their opinion registered early on that heart disease was due to high-fat diets leading to high cholesterol. Decades later, scientists are still trying to overcome the effects of that extremely motivated reasoning.
What Doctors Must Do to Rebuild Faith:
Once trust is broken, a lot of care is required to repair it. Honesty, integrity, transparency and validation must all be part of the conversation. And both sides must avoid motivated reasoning as much as possible!
Patients can help doctors in the course of diagnosis by asking, “What else could this be?” That encourages a consideration of differential diagnoses and the possibility that the first guess might not be right. According to Dr. Wilson, we should all entertain the idea of medicine as a team sport and look for ways to form a therapeutic alliance with those charged with helping us heal.
This Week's Guest:
F. Perry Wilson, MD, is a nephrologist, epidemiologist, and associate professor at Yale School of Medicine. His research focuses on using data and analytics to personalize medicine for each individual. He is the director of Yale Clinical and Translational Research Accelerator (CTRA) and co-director of the Yale Section of Nephrology Human Genetics and Clinical Research Core. He’s a columnist at Medscape where he hosts a popular series called “The Impact Factor,” which analyzes the strengths and weaknesses of published studies. Dr. Wilson is the author of How Medicine Works and When It Doesn't: Learning Who to Trust to Get and Stay Healthy.
[caption id="attachment_130504" align="alignnone" width="1024"]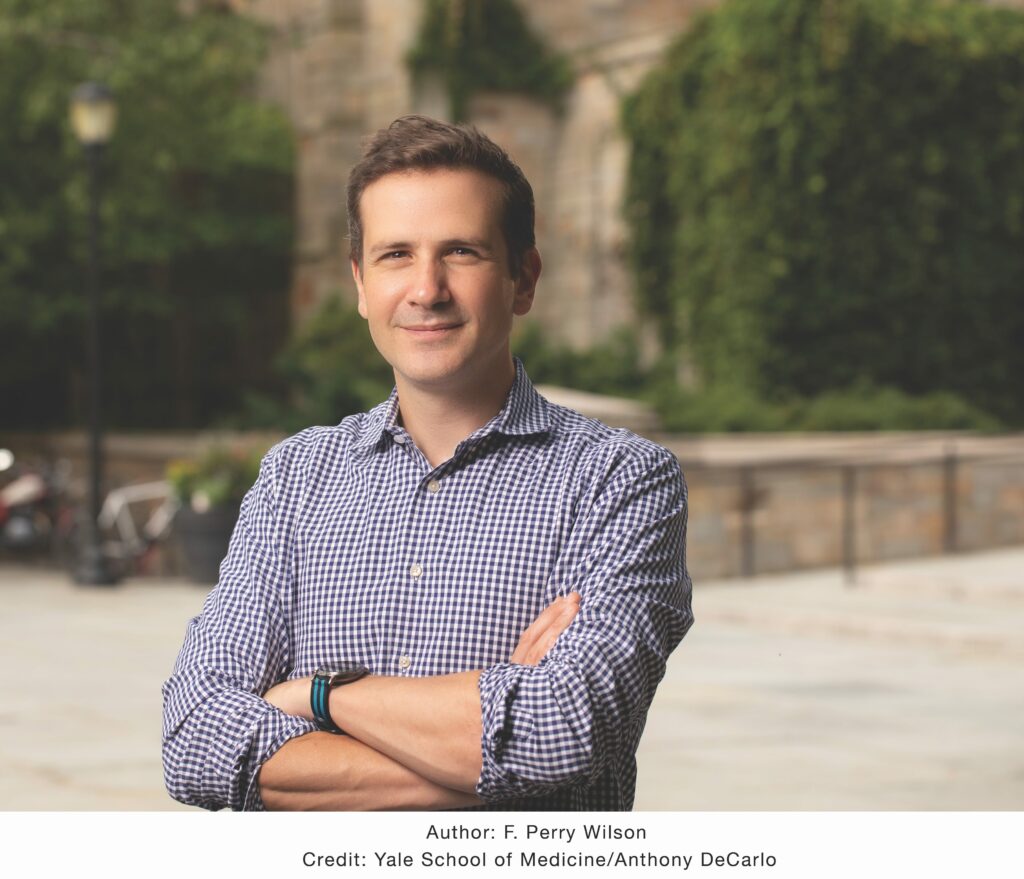 2020-08-13 Dr. Francis Wilson. Photo Credit Anthony DeCarlo[/caption]
2020-08-13 Dr. Francis Wilson. Photo Credit Anthony DeCarlo[/caption]